Stroke Medicine
Stroke is the fourth commonest cause of death and the largest cause of adult neurological disability in the UK. From a socioeconomic perspective the disease is estimated to cost approximately £9 billion pounds per annum because of long term care expenditure, medical and rehabilitation needs and loss of employment. Such as its importance, it has been identified as one of the sentinel conditions in the NHS Long Term Plan.
Stroke Mediicne is a fantastic training opportunity within a clinical specialty that deals with a wide range of transferable training elements; internal medicine, neurology, palliative care, rehabilitation etc and fosters a consultant career with excellent employability spanning a number of decades. Currently Stroke Medicine is a sub-specialty training programme open to trainees holding a medical specialty national training number (NTN) in Acute Internal Medicine, Cardiology, Clinical Pharmacology and Therapeutics, Geriatric Medicine, Neurology and Rehabilitation Medicine. Although 2 years of training is required, the first year is generally delivered within the parent specialty programme followed by an advanced training year. This advanced year is usually taken in the penultimate year of training to gain the most benefit from the year (but can be taken at any stage in higher specialty training) and the regional programmes are outlined below. Stroke medicine sub-specialty accreditation is an additional qualification where successful prospective completion of such training leads to subspecialty of Stroke Medicine in their entry on the GMC’s specialist register after the award of a CCT in their parent specialty.
The primary purpose of sub-specialty training in stroke is to promote the development of physicians with the knowledge, skills and attitudes to function as an expert consultant resource within specialist stroke services.
The future structure of training in stroke medicine is currently under review; driven by the implementation of the Internal Medicine curriculum and planned changes to the higher training curricula from 2022.
It is strongly recommended that trainees who are interested in Stroke Medicine accreditation should discuss this with the Training Programme Director (TPD) for both Stroke and their parent specialty early in their training.
Recruitment to stroke medicine subspecialty training is now through the national recruitment process. This can be found at: https://www.st3recruitment.org.uk
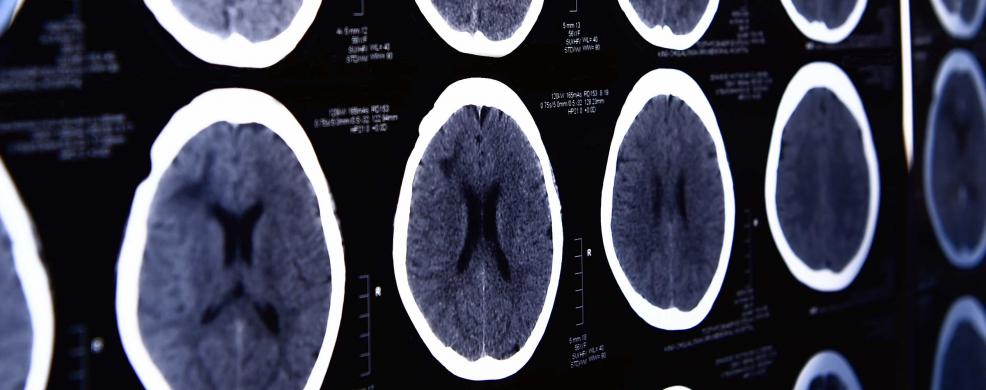
Within Health Education England working across Yorkshire and the Humber there are four training posts at approved training centres in Hull University Teaching Hospital (one post), Leeds Teaching Hospitals NHS Trust (one post), Sheffield Teaching Hospitals NHS Foundation Trust (two posts). There are other hospital trusts in the region that have GMC approval for training; allowing flexibility for training should any additional / Trust funding become available. Each provides the infrastructure to deliver high quality training in cerebrovascular medicine; (hyper) acute stroke, stroke rehabilitation, secondary prevention and also insight into service development / provision either within one centre or across sites and research. To accommodate experience in all aspects of stroke and advancing technologies, experience in larger centers may be necessary.
We currently run a 'fellowship model' where advanced stroke training is delivered over one year and is designed around the needs of the trainee depending upon their parent specialty, with the aim to develop physicians with the attributes to run a specialist stroke service. After satisfactory completion of training, trainees will be accredited with the subspecialty of Stroke Medicine on the GMC specialist register following the award of their parent specialty CCT.
Further information including curriculum, assessments and downloads can be found on the JRCPTB site.